- +91 80 41509150
- info@pearloptics.in
Good eye health and eye care are crucial to the value of sight. Be proactive in your eye health by taking a role in maintaining and protecting your sight, preventing common eye disorders, and treating problems early. Eye-care professionals, including ophthalmologists (medical doctors specializing in diseases and surgery of the eye) and optometrists recommend that everyone with visual or other eye signs or symptoms have their eyes checked. In people who have no symptoms, it is recommended that people over 40 have their eyes checked every two years and people over 60 have their eyes checked annually.
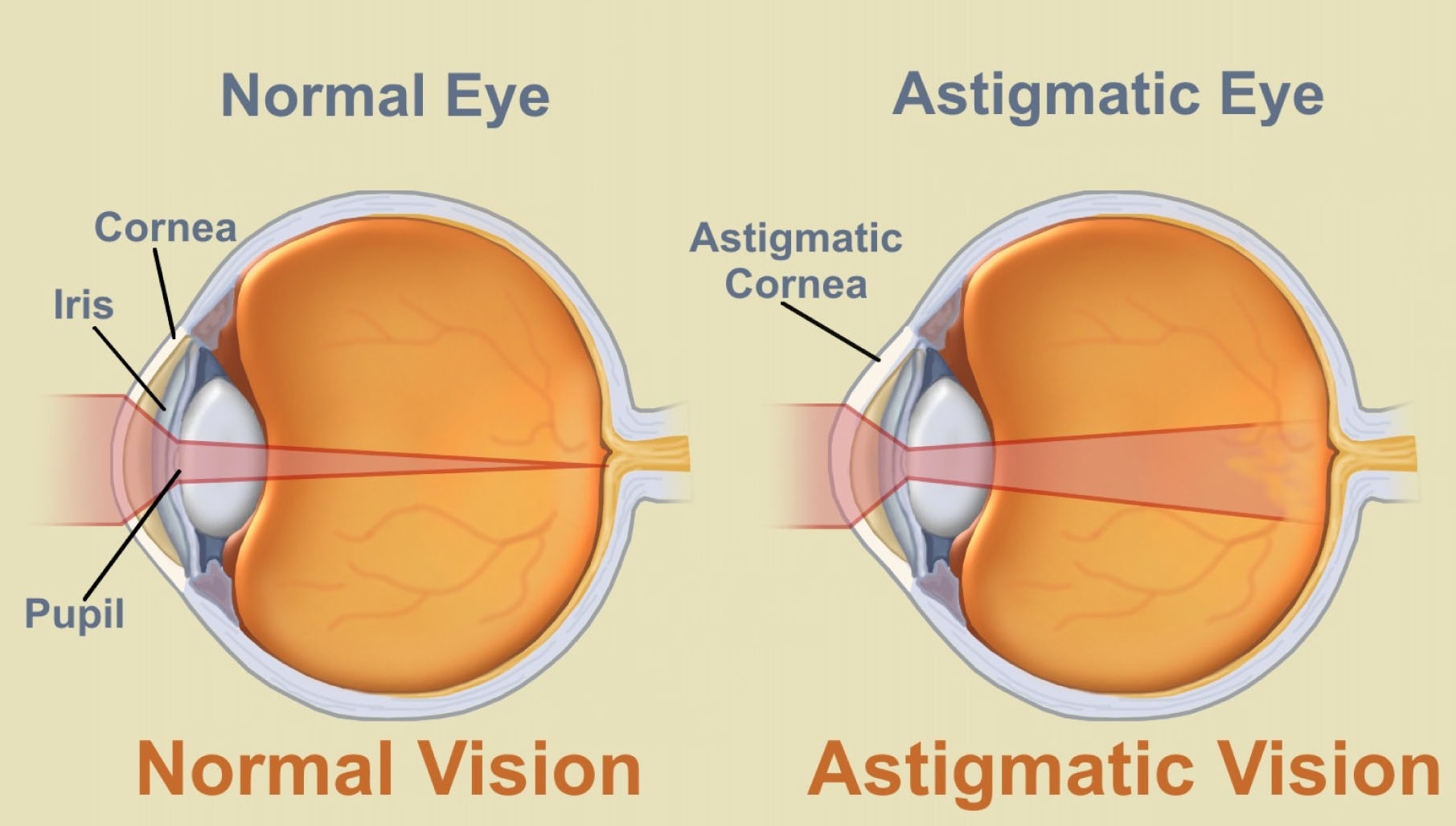 Astigmatism is an optical defect in which vision is blurred due to the inability of the optics of the eye to focus a point object into a sharp focused image on the retina. This may be due to an irregular or toric curvature of the cornea or lens. There are two types of astigmatism: regular and irregular. Irregular astigmatism is often caused by a corneal scar or scattering in the crystalline lens and cannot be corrected by standard spectacle lenses, but can be corrected by contact lenses. Regular astigmatism arising from either the cornea or crystalline lens can be corrected by a toric lens. A toric surface resembles a section of the surface of an American football or a doughnut where there are two regular radii, one smaller than another. This optical shape gives rise to regular astigmatism in the eye.
Astigmatism is an optical defect in which vision is blurred due to the inability of the optics of the eye to focus a point object into a sharp focused image on the retina. This may be due to an irregular or toric curvature of the cornea or lens. There are two types of astigmatism: regular and irregular. Irregular astigmatism is often caused by a corneal scar or scattering in the crystalline lens and cannot be corrected by standard spectacle lenses, but can be corrected by contact lenses. Regular astigmatism arising from either the cornea or crystalline lens can be corrected by a toric lens. A toric surface resembles a section of the surface of an American football or a doughnut where there are two regular radii, one smaller than another. This optical shape gives rise to regular astigmatism in the eye.

Blepharitis is an inflammation of the eyelids causing red, irritated, itchy eyelids and the formation of dandruff-like scales on eyelashes. It is a common eye disorder caused by either bacterial or a skin condition such as dandruff of the scalp or acne rosacea. It affects people of all ages. Although uncomfortable, blepharitis is not contagious and generally does not cause any permanent damage to eyesight. Individuals with blepharitis may experience a gritty or burning sensation in their eyes, excessive tearing, itching, red and swollen eyelids, dry eyes, or crusting of the eyelids. For some people, blepharitis causes only minor irritation and itching. However, it can lead to more severe signs and symptoms such as blurring of vision, missing or misdirected eyelashes, and inflammation of other eye tissue, particularly the cornea.
In many cases, good eyelid hygiene and a regular cleaning routine can control blepharitis. This includes frequent scalp and face washing, using warm compresses to soak the eyelids, and doing eyelid scrubs. In cases where a bacterial infection is the cause, various antibiotics and other medications may be prescribed along with eyelid hygiene.
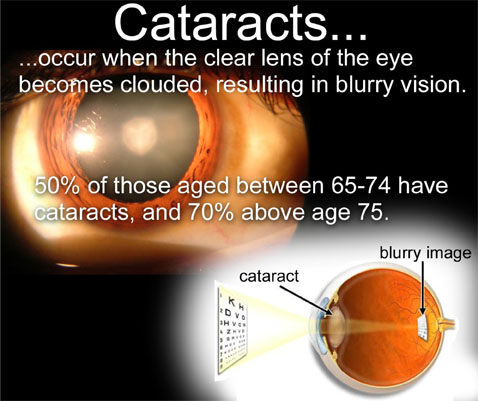
Cataract is a painless condition where the normally clear aspirin-sized lens of the eye starts to become cloudy. The result is much like smearing grease over the lens of a camera which impairs normal vision. Causes of cataracts include cortisone medication, trauma, diabetes, and aging.
In fact, cataracts will affect most people if they live long enough. Diagnosis can be made when an optometrist examines the eyes with a viewing instrument. Symptoms of early cataracts may be improved with new eyeglasses, brighter lighting, anti-glare sunglasses, or magnifying lenses. If these measures do not help, surgically removing the cloudy lens and replacing it with an artificial lens is the only effective treatment. Removal is only necessary when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. Consult an ophthalmologist for cataract removal.

A chalazion is a tiny lump of the upper or lower eyelid caused by inflammation of a gland of the lid. It may be soft and fluid-filled or firmer.
A chalazion is also referred to as a meibomian cyst, tarsal cyst, or conjunctival granuloma.
The narrow opening through which a meibomian gland secretes its material can become clogged from narrowing of the opening or hardening of the sebaceous liquid near the opening. If this occurs, the gland will have a backup of the material it secretes and it will swell. Most chalazions are treated with warm compresses to the eyelid to promote healing and circulation of blood to the inflamed area.
Doctors may prescribe an antibiotic drop or ointment to be used immediately after the compresses. If the chalazion persists and is causing an unsightly lump, it can be removed surgically through the inside of the lid.
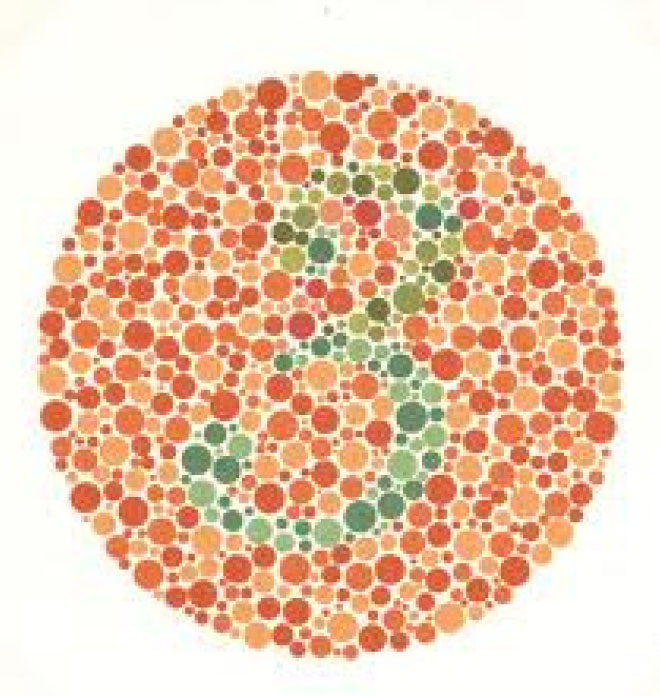
Color blindness or color vision deficiency is the inability to distinguish certain shades of color or in more severe cases, see colors at all. The term "color blindness" is also used to describe this visual condition, but very few people are completely color blind Most people with color vision deficiency can see colors, but they have difficulty differentiating between
-> particular shades of reds and greens (most common) or
-> blues and yellows (less common).
People who are totally color blind, a condition called achromatopsia, can only see things as black and white or in shades of gray
Conjunctivitis is an inflammation or infection of the conjunctiva, the thin transparent layer of tissue that lines the inner surface of the eyelid and covers the white part of the eye. Conjunctivitis, often called “pink eye,” is a common eye disease, especially in children. It may affect one or both eyes. Some forms of conjunctivitis can be highly contagious and easily spread in schools and at home. While conjunctivitis is usually a minor eye infection, sometimes it can develop into a more serious problem.
Conjunctivitis may be caused by a viral or bacterial infection. It can also occur due to an allergic reaction to irritants in the air like pollen and smoke, chlorine in swimming pools, and ingredients in cosmetics or other products that come in contact with the eyes. Sexually transmitted diseases like Chlamydia and gonorrhea are less common causes of conjunctivitis.
 People with conjunctivitis may experience the following symptoms:
People with conjunctivitis may experience the following symptoms:
-> A gritty feeling in one or both eyes
-> Itching or burning sensation in one or both eyes
-> Excessive tearing
-> Discharge coming from one or both eyes
-> Swollen eyelids
-> Pink discoloration to the whites of one or both eyes
-> Increased sensitivity to light
Types of Conjunctivitis:
Since the term Conjunctivitis is a broad term, there are specific types when discussing this condition.
There are three main types of Conjunctivitis.
1. Allergic Conjunctivitis
2. Infectious Conjunctivitis (This form is caused by bacteria and viruses.)
3. Chemical Conjunctivitis
Most corneal ulcers are caused by infections and can be bacterial (common in people who wear contact lenses), viral herpes simplex virus and varicella virus, or fungal (improper care of contact lenses or overuse of eye drops that contain steroids).
Symptoms include red eyes, pain, feeling like something is in the eye, tearing, pus/thick discharge, blurry vision, pain from bright lights, swollen eyelids, or a white or gray round spot on the cornea.
Self-treatment consists of removing contact lenses, applying a cool compress to the affected eye and washing hands often.
Anyone with a corneal ulcer should be seen immediately by an ophthalmologist, who will do testing and most likely prescribe antibiotic and other eye drops. If the ulcer persists or worsens, a surgical procedure known as corneal transplantation may be performed.
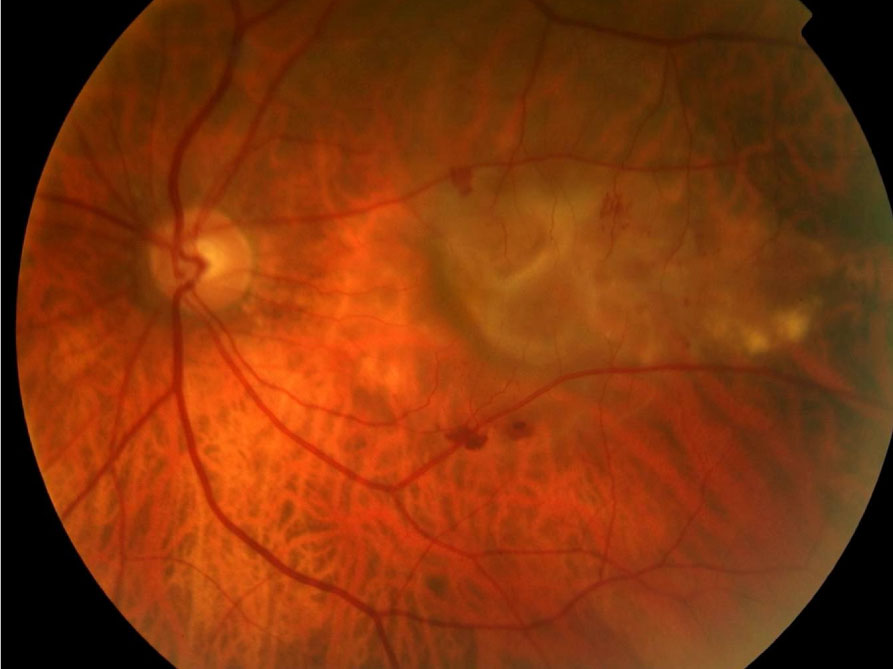
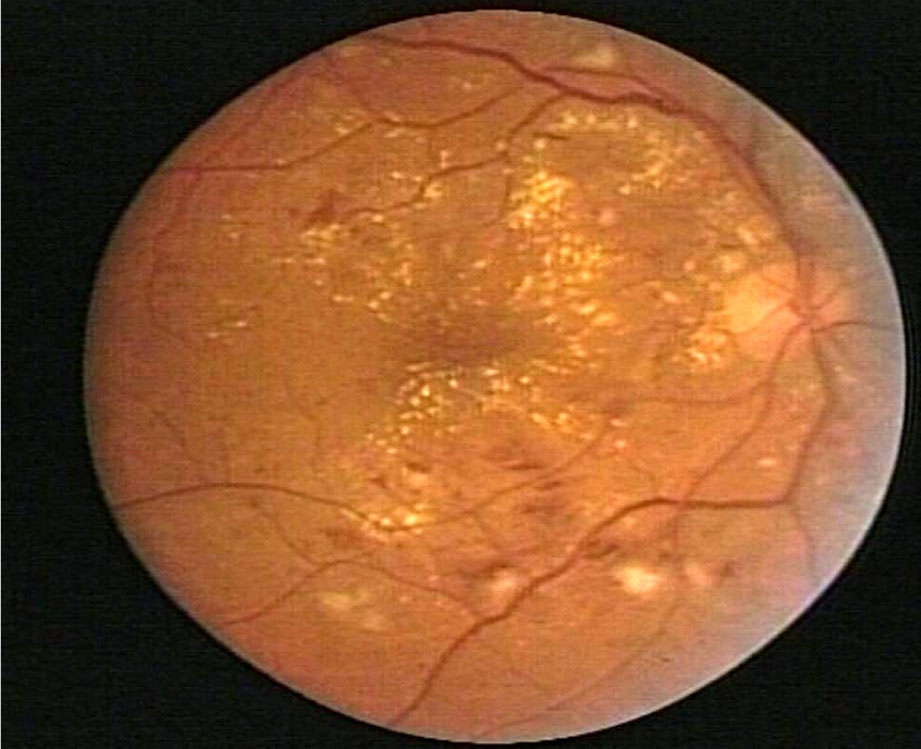
Diabetic retinopathy is a condition occurring in persons with diabetes, which causes progressive damage to the retina, the light sensitive lining at the back of the eye. It is a serious sight-threatening complication of diabetes.
Diabetes is a disease that interferes with the body's ability to use and store sugar, which can cause many health problems. Too much sugar in the blood can cause damage throughout the body, including the eyes. Over time, diabetes affects the circulatory system of the retina.
Diabetic retinopathy is the result of damage to the tiny blood vessels that nourish the retina. They leak blood and other fluids that cause swelling of retinal tissue and clouding of vision. The condition usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness.
 Symptoms of diabetic retinopathy include:
Symptoms of diabetic retinopathy include:
-> Seeing spots or floaters in your field of vision
-> Blurred vision
-> Having a dark or empty spot in the center of your vision
-> Difficulty seeing well at night
Often there are no visual symptoms in the early stages of diabetic retinopathy. That is why the American Optometric Association recommends that everyone with diabetes have a comprehensive dilated eye examination once a year. Early detection and treatment can limit the potential for significant vision loss from diabetic retinopathy.
If you are a diabetic, you can help prevent or slow the development of diabetic retinopathy by taking your prescribed medication, sticking to your diet, exercising regularly, controlling high blood pressure and avoiding alcohol and smoking.

Severe allergic eye symptoms can be very distressing and are a common reason for visits to the allergist or ophthalmologist. Occasionally, severe eye allergies cause serious damage that can threaten eyesight.
Eye allergies usually are associated with other allergic conditions, particularly hay fever (allergic rhinitis) and atopic eczema (dermatitis). Medications and cosmetics can also play a significant role in causing eye allergies. You should seek medical advice.
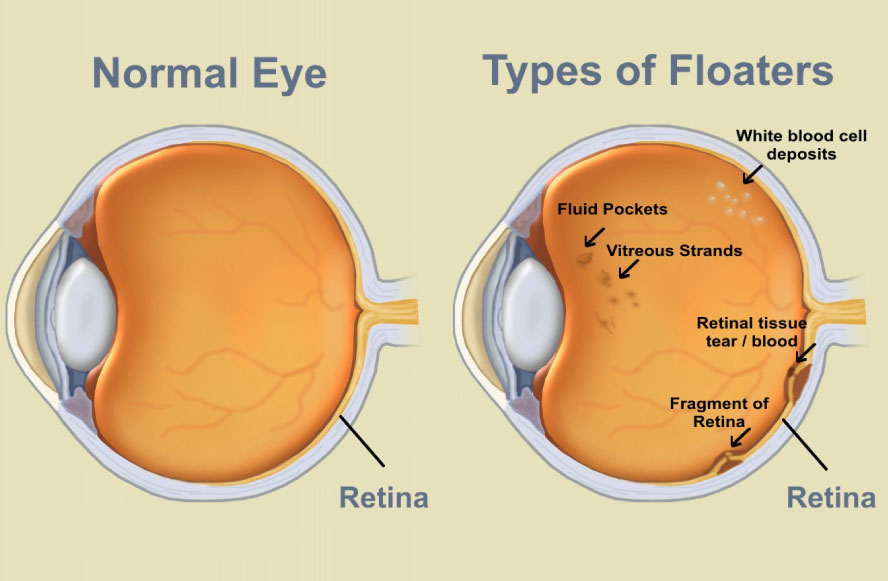
Floaters are deposits of various size, shape, consistency, refractive index, and motility within the eye's vitreous humour, which is normally transparent. They may be of embryonic origin or acquired due to degenerative changes of the vitreous humour or retina Floaters are visible because of the shadows they cast on the retina or their refraction of the light that passes through them, and can appear alone or together with several others in one's field of vision. They may appear as spots, threads, or fragments of cobwebs, which float slowly before the observer's eyes. Since these objects exist within the eye itself, they are not optical illusions but are entoptic phenomena.
Most spots are not harmful and rarely limit vision. But, spots can be indications of more serious problems, and you should see your optometrist or ophthalmologist for a comprehensive examination when you notice sudden changes or see increases in them.
By looking in your eyes with special instruments, your optometrist or ophthalmologist can examine the health of your eyes and determine if what you are seeing is harmless or the symptom of a more serious problem that requires treatment.
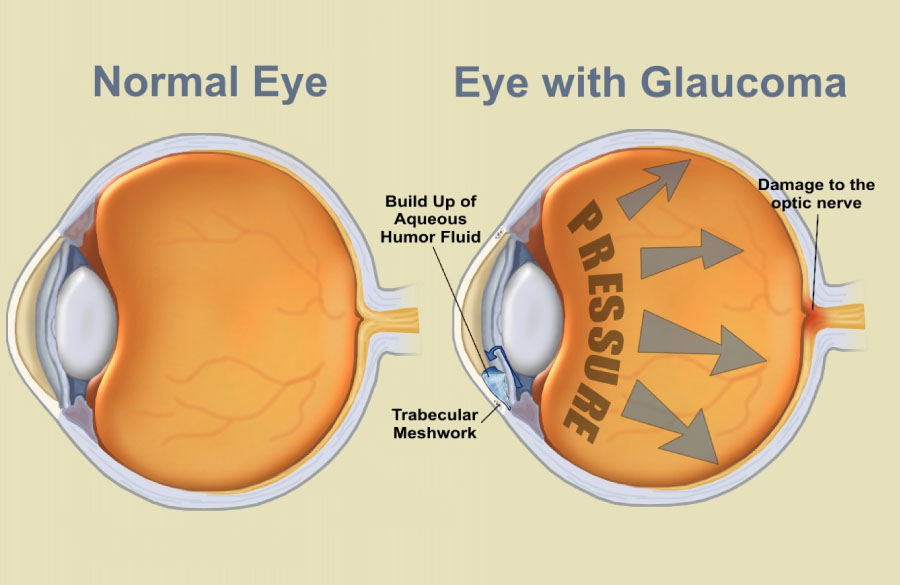
Glaucoma is an eye disorder in which the optic nerve suffers damage, permanently impacting vision in the affected eye(s) and progressing to complete blindness if untreated. It is often, but not always, associated with increased pressure of the fluid in the eye (aqueous humour).
Glaucoma has been nicknamed the "silent thief of sight" because the loss of vision normally occurs gradually over a long period of time and is often only recognized when the disease is quite advanced. Once lost, this damaged visual field cannot be recovered. Worldwide, it is the second leading cause of blindness. Glaucoma affects 1 in 200 people aged fifty and younger, and 1 in 10 over the age of eighty. If the condition is detected early enough it is possible to arrest the development or slow the progression with medical and surgical means. A constant evaluation with the opthalmologist is advised.
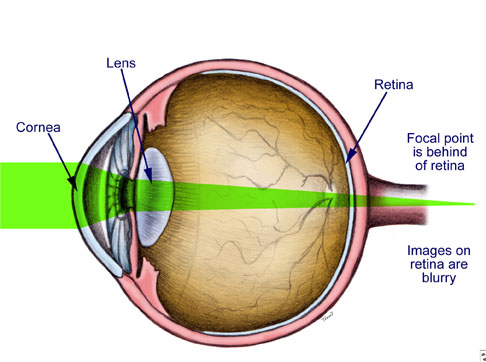
Hyperopia, also known as farsightedness, longsightedness or hypermetropia, is a defect of vision caused by an imperfection in the eye (often when the eyeball is too short or the lens cannot become round enough), causing difficulty focusing on near objects, and in extreme cases causing a sufferer to be unable to focus on objects at any distance. As an object moves toward the eye, the eye must increase its optical power to keep the image in focus on the retina. If the power of the cornea and lens is insufficient, as in hyperopia, the image will appear blurred.
The causes of hyperopia are typically genetic and involve an eye that is too short or a cornea that is too flat, so that images focus at a point behind the retina. People with hyperopia can usually see distant objects well, but have trouble focusing on nearby objects.

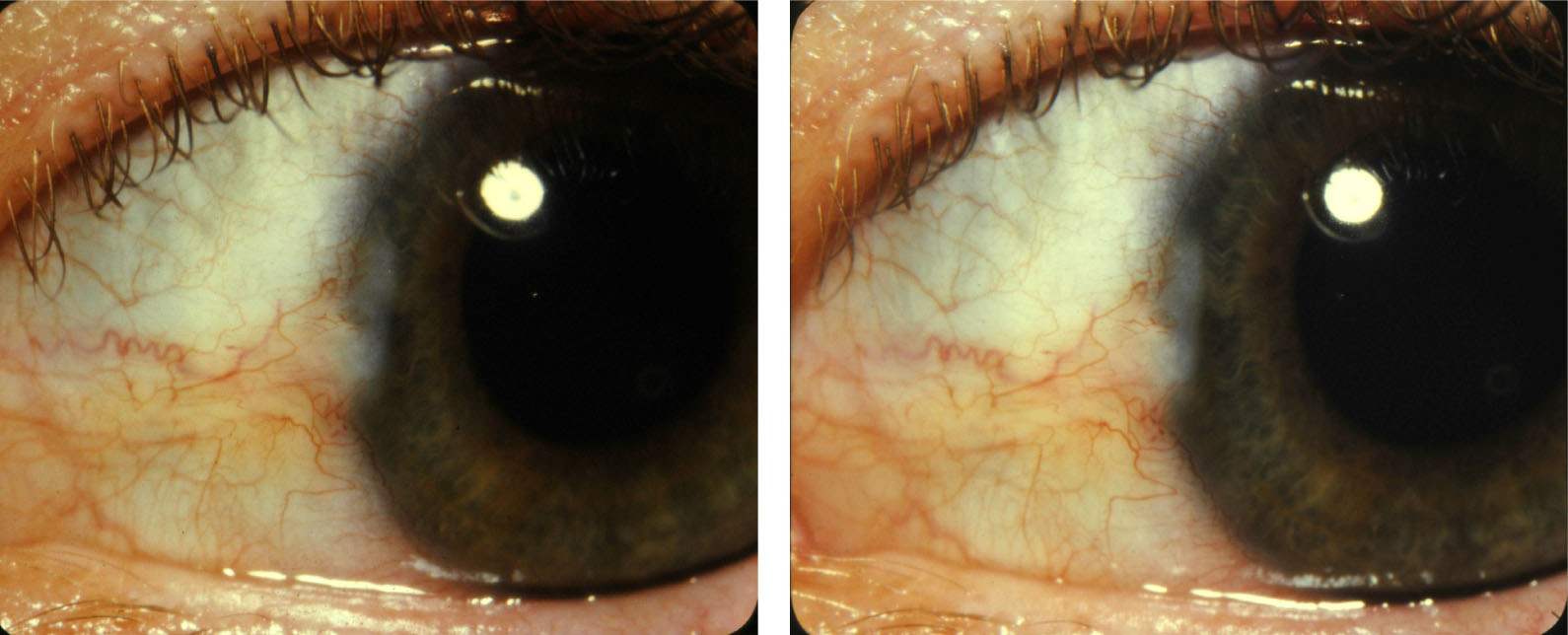
Keratoconus is a degenerative disorder of the eye in which structural changes within the cornea cause it too thin and change to a more conical shape than its normal gradual curve.
Keratoconus can cause substantial distortion of vision, with multiple images, streaking and sensitivity to light all often reported by the patient. It is typically diagnosed in the patient's adolescent years and attains its most severe state in the twenties and thirties. If afflicting both eyes, the deterioration in vision can affect the patient's ability to drive a car or read normal print. In most cases, corrective RGP Contact lenses are effective enough to allow the patient to continue to drive legally and likewise function normally. Further progression of the disease may require surgery including intrastromal cornea ring segments, corneal collagen cross-linking, or corneal transplantation. However, despite the disease's unpredictable course, keratoconus can often be successfully managed with little or no impairment to the patient's quality of life.
Keratoconus affects around one person in a thousand. It seems to occur in populations throughout the world, although it occurs more frequently in certain ethnic groups.The exact cause of keratoconus is uncertain, but has been associated with detrimental enzyme activity within the cornea. A genetic link seems likely, as the incidence rate is greater if a family member has been diagnosed.
We proudly present the most experienced optometrist who will help you in achieving the best vision with the help of a large variety of RGP contact lenses. You can be assured of comfortable vision in your daily routine life.
Age related macular degeneration is a medical condition which usually affects older adults that results in a loss of vision in the center of the visual field (the macula) because of damage to the retina. It occurs in “dry” and “wet” forms. It is a major cause of visual impairment in older adults (>50 years). Macular degeneration can make it difficult or impossible to read or recognize faces, although enough peripheral vision remains to allow other activities of daily life. Consulting an opthalmologist on a regular basis will be helpful.
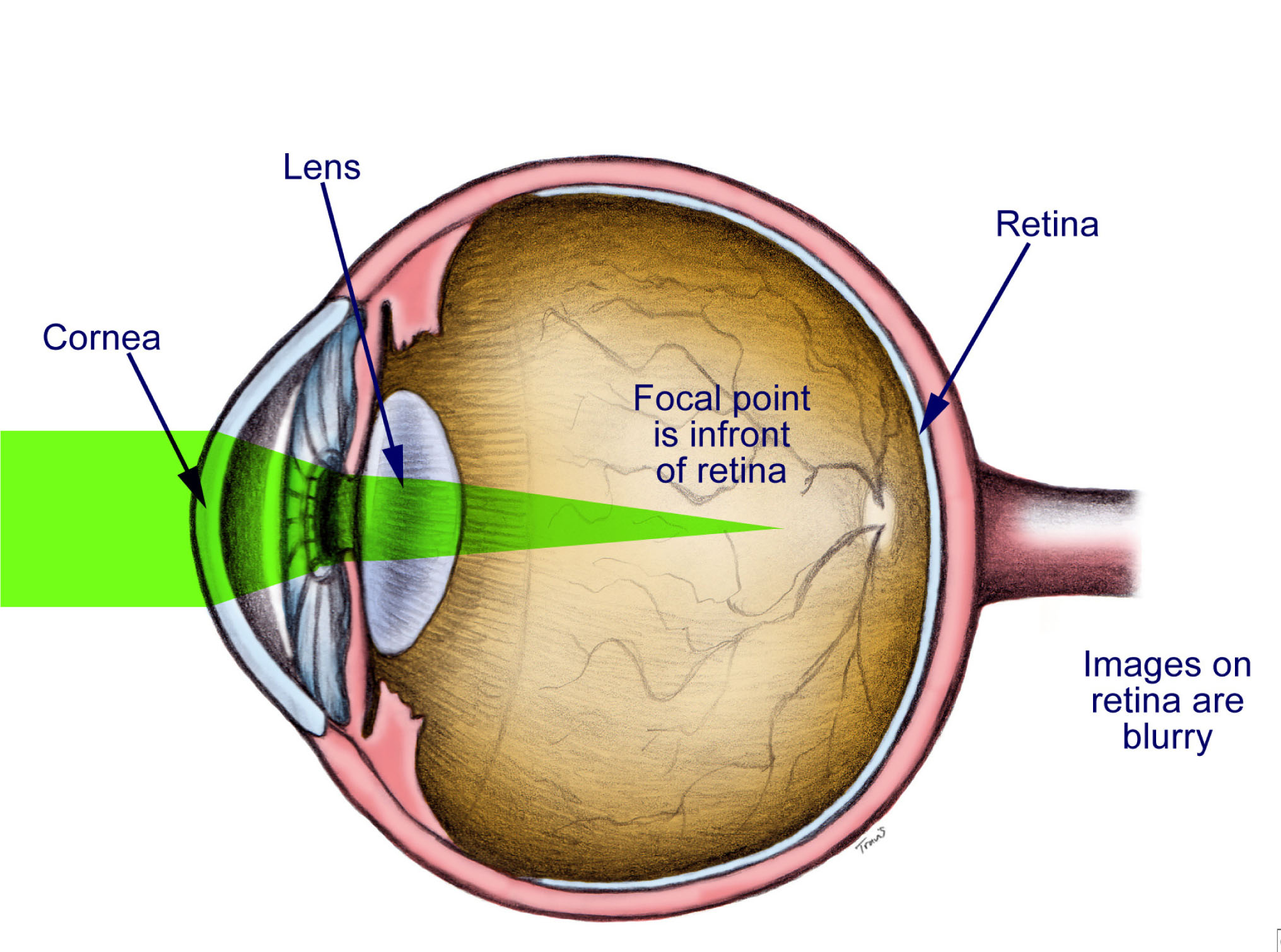
Myopia also known as farsightedness is a refractive condition of the eye in which collimated light produces image focus in front of the retina when accommodation is relaxed. Myopia is the medical term for nearsightedness. People with myopia see objects more clearly when they are close to the eye, while distant objects appear blurred or fuzzy. Reading and close-up work may be clear, but distance vision is blurry.
Eye care professionals most commonly correct myopia through the use of corrective lenses, such as glasses or contact lenses. It may also be corrected by refractive surgery, but this does have certain risks and side effects. The corrective lenses have a negative optical power (i.e. are concave) which compensates for the excessive positive diopters of the myopic eye.
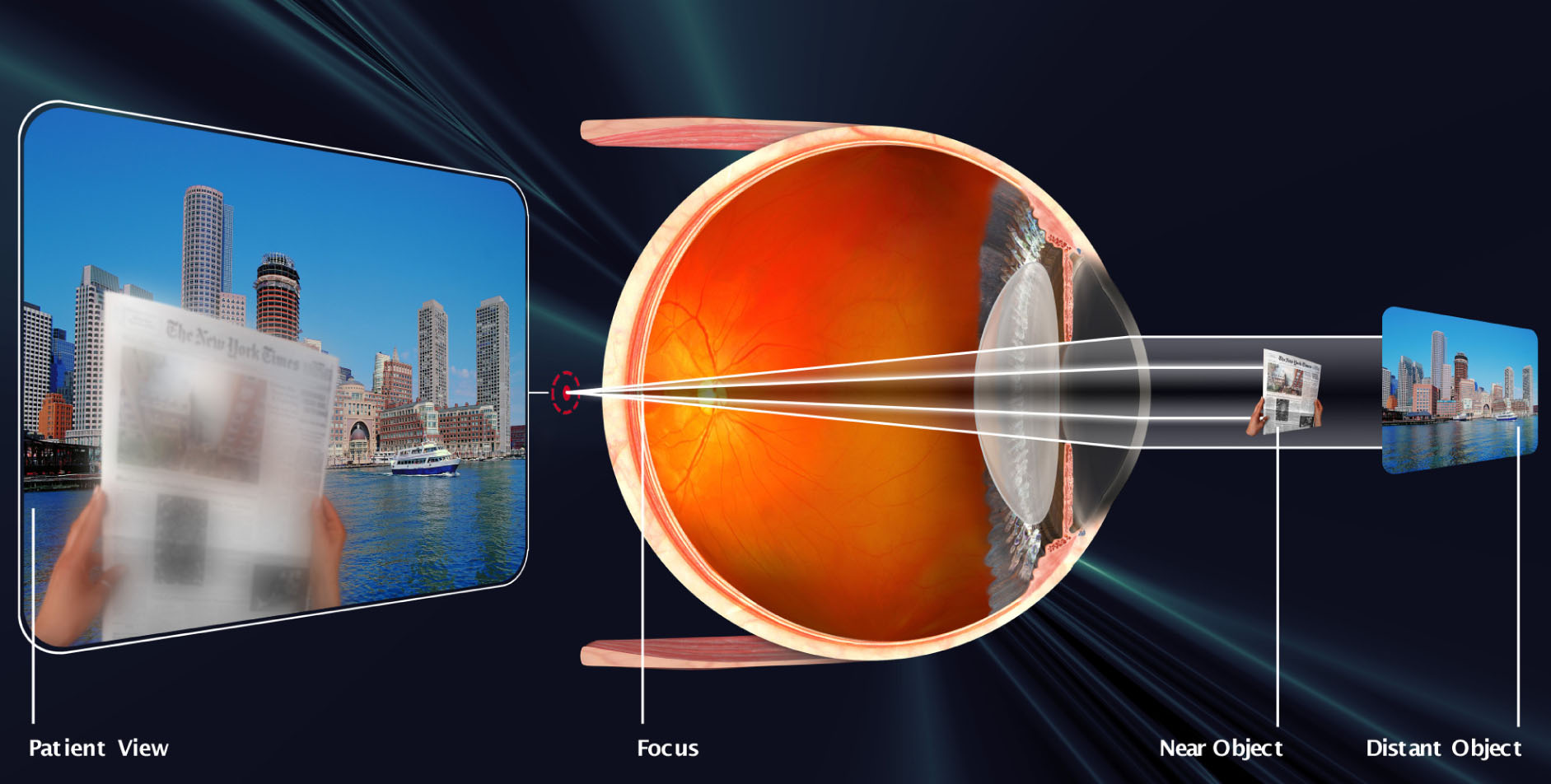
Presbyopia is a vision condition in which the crystalline lens of your eye loses its flexibility, which makes it difficult for you to focus on close objects.Presbyopia may seem to occur suddenly, but the actual loss of flexibility takes place over a number of years. Presbyopia usually becomes noticeable in the early to mid-40s and is a natural part of the aging process of the eye. It is not a disease, and it cannot be preventedSome signs of presbyopia include the tendency to hold reading materials at arm's length, blurred vision at normal reading distance and eye fatigue along with headaches when doing close work. A comprehensive optometric examination will include testing for presbyopia.To help you compensate for presbyopia, your optometrist can prescribe reading glasses, bifocals, trifocals or contact lenses
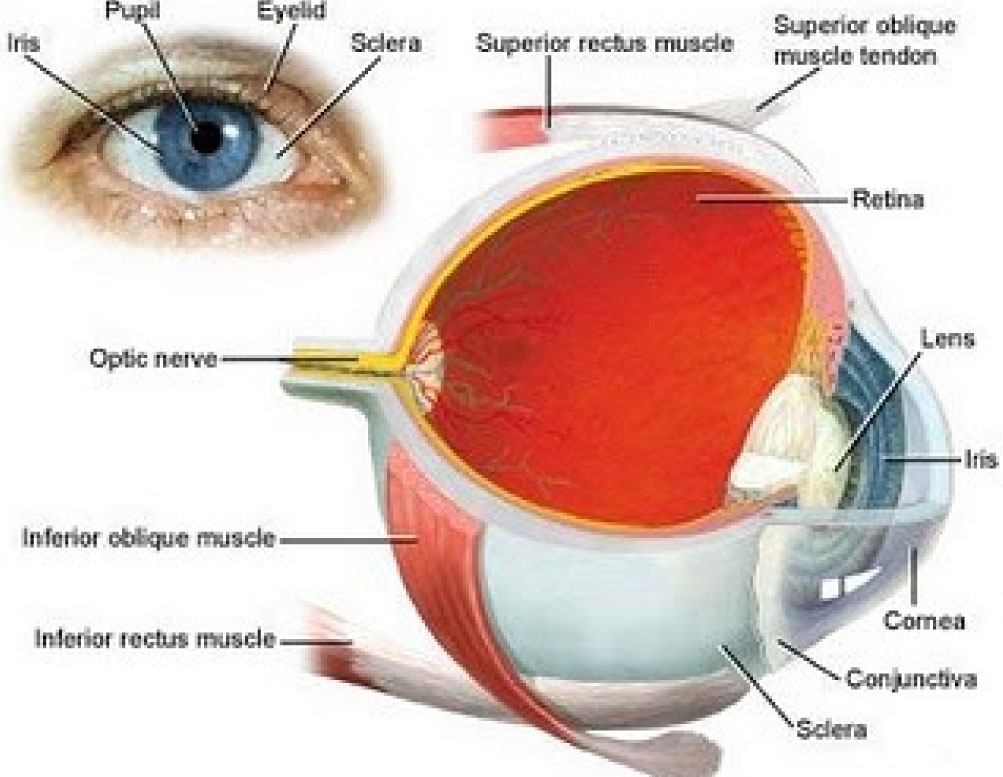
Good eye health and eye care are crucial to the value of sight. Be proactive in your eye health by taking a role in maintaining and protecting your sight, preventing common eye disorders, and treating problems early.
Eye-care professionals, including ophthalmologists (medical doctors specializing in diseases and surgery of the eye) and optometrists recommend that everyone with visual or other eye signs or symptoms have their eyes checked.
In people who have no symptoms, it is recommended that people over 40 have their eyes checked every two years and people over 60 have their eyes checked annually.
Pterygium most often refers to a benign growth of the conjunctiva. A pterygium commonly grows from the nasal side of the sclera. It is associated with, and thought to be caused by ultraviolet-light exposure (e.g. sunlight), low humidity, and dust. An opthalmologist will be able to guide you regarding the protection and prevention of further progress.

Ptosis is a (drooping) of the upper or lower eyelid. The drooping may be worse after being awake longer, when the individual's muscles are tired. If severe enough and left untreated, the drooping eyelid can cause other conditions, such as amblyopia or astigmatism. This is why it is especially important for this disorder to be treated in children at a young age, before it can interfere with vision development. Please consult an opthalmologist for the best remedy.
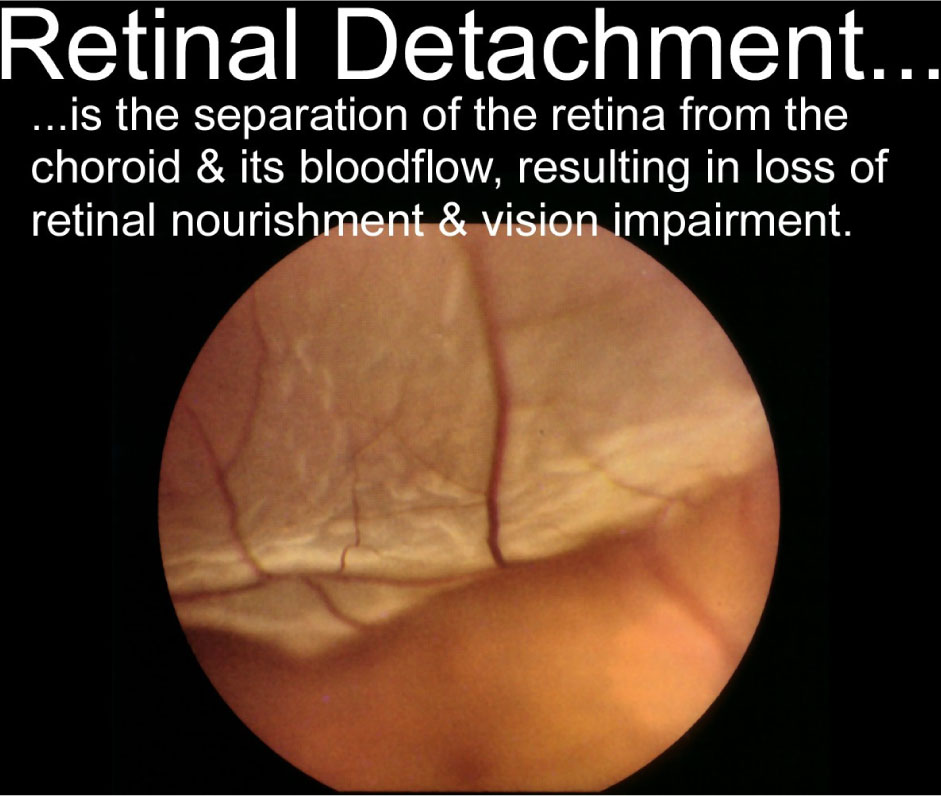
Retinal detachment is a disorder of the eye in which the retina peels away from its underlying layer of support tissue. Initial detachment may be localized, but without rapid treatment the entire retina may detach, leading to vision loss and blindness. The retina is a thin layer of light sensitive tissue on the back wall of the eye. The optical system of the eye focuses light on the retina much like light is focused on the film in a camera. The retina translates that focused image into neural impulses and sends them to the brain via the optic nerve. Occasionally, posterior vitreous detachment, injury or trauma to the eye or head may cause a small tear in the retina. The tear allows vitreous fluid to seep through it under the retina, and peel it away like a bubble in wallpaper.
IT IS A MEDICAL EMERGENCY AND YOU NEED TO CONSULT AN OPTHALMOLOGIST IMMEDIATELY.
Retinitis pigmentosa (RP) is a group of inherited diseases that damage the light-sensitive rods and cones located in the retina, the back part of our eyes. Rods, which provide side (peripheral) and night vision are affected more than the cones that provide color and clear central vision.
Signs of RP usually appear during childhood or adolescence. The first sign is often night blindness followed by a slow loss of side vision. Over the years, the disease will cause further loss of side vision. As the disease develops, people with RP may often bump into chairs and other objects as side vision worsens and they only see in one direction - straight ahead. They see as if they are in a tunnel (thus the term tunnel vision).
Fortunately, most cases of retinitis pigmentosa take a long time to develop and vision loss is gradual. It may take many years for loss of vision to be severe.
Currently, there is no cure for RP, but there is research that indicates that vitamin A and lutein may slow the rate at which the disease progresses. Your doctor of optometry can give you more specific information on nutritional supplements that may help you.
Also, there are many new low vision aids, including telescopic and magnifying lenses, night vision scopes as well as other adaptive devices, that are available that help people maximize the vision that they have remaining. An optometrist, experienced in low vision rehabilitation, can provide these devices as well as advice about other training and assistance to help people remain independent and productive.
Becuase it is an inherited disease, research into genetics may one day provide a prevention or cure for those who have RP.

Crossed eyes or Strabismus as it is medically termed, is a condition in which both eyes do not look at the same place at the same time. It occurs when an eye turns in, out, up or down and is usually caused by poor eye muscle control or a high amount of farsightedness.
There are six muscles attached to each eye that control how it moves. The muscles receive signals from the brain that direct their movements. Normally, the eyes work together so they both point at the same place. When problems develop with eye movement control, an eye may turn in, out, up or down. The eye turning may be evident all the time or may appear only at certain times such as when the person is tired, ill, or has done a lot of reading or close work. In some cases, the same eye may turn each time, while in other cases, the eyes may alternate turning.
Maintaining proper eye alignment is important to avoid seeing double, for good depth perception, and to prevent the development of poor vision in the turned eye. When the eyes are misaligned, the brain receives two different images.
Strabismus is classified by the direction the eye turns:
-> Inward turning is called esotropia
-> Outward turning is called exotropia
-> Upward turning is called hypertropia
-> Downward turning is called hypotropia
Treatment for strabismus may include eyeglasses, prisms, vision therapy, or eye muscle surgery. If detected and treated early, strabismus can often be corrected with excellent results.

An external stye or hordeolum is an infection of the sebaceous glands of Zeis at the base of the eyelashes, or an infection of the apocrine sweat glands of Moll External styes form on the outside of the lids and can be seen as small red bumps. Internal styes are infections of the meibomian sebaceous glands lining the inside of the eyelids. They also cause a red bump underneath the lid with only generalized redness and swelling visible on the outside. Styes are characterized by an acute onset and usually short in duration (7–10 days without treatment) and it is advised to see your opthalmologist in case irritation persists.